Infantile colic is a common disorder of gut-brain interaction, affecting approximately 20-30% of infants during the first months of life. It is typically benign and self-limiting, but excessive crying often leads to medical consultations and significant parental distress. Although cow’s milk allergy (CMA) is frequently considered in the differential diagnosis, its role in infantile colic remains limited and should be interpreted with caution, particularly when colic occurs as an isolated symptom.
This narrative review critically evaluates the available evidence on the association between infantile colic and CMA, with the aim of clarifying when CMA should (and should not) be suspected in clinical practice.
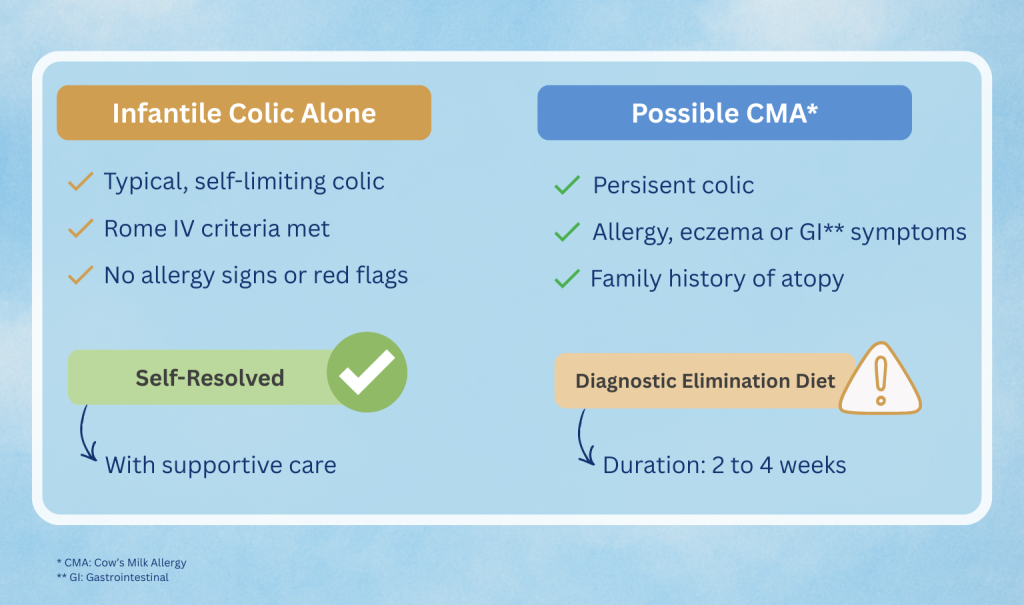
Overview of clinical scenarios in infantile colic and selective consideration of cow’s milk allergy based on associated symptoms.
Key Clinical Insights
Based on a review of 135 publications, including 18 clinical trials assessing cow’s milk elimination diets, the authors conclude that infantile colic alone is rarely caused by CMA. Given the high prevalence of colic and the much lower prevalence of CMA, excessive crying in isolation has low diagnostic value for CMA.
The evidence indicates that CMA may contribute to symptoms only in a subset of infants, particularly when colic is not an isolated finding but occurs as part of a broader clinical picture suggestive of allergy. In these cases, crying is considered one component of a multisystem presentation, rather than a standalone manifestation of CMA.
CMA should be considered when infantile colic:
- Persists despite appropriate reassurance, parental education, and general supportive measures
- Is accompanied by additional symptoms suggestive of allergy, such as eczema, persistent regurgitation or vomiting, diarrhea, constipation, blood or mucus in stools, or faltering growth
- Occurs in infants with a family history of atopy
When CMA is suspected on clinical grounds, a time-limited diagnostic elimination diet is recommended:
- A 2-4-week maternal cow’s milk elimination diet for breastfed infants, with attention to maternal nutritional adequacy
- A 2-4-week trial of an extensively hydrolyzed cow’s milk formula (or suitable alternative) for formula-fed infants
If symptoms improve during elimination, reintroduction of cow’s milk protein is mandatory to confirm or exclude the diagnosis, as there is no reliable laboratory test for non-IgE-mediated CMA. Improvement during elimination alone is insufficient to establish causality.
Routine allergy testing (skin prick testing or serum IgE) is not recommended in infants with isolated colic unless IgE-mediated CMA is suspected. Awareness tools such as the Cow’s Milk-related Symptom Score (CoMiSS™) may help identify infants who warrant further evaluation, but should not be used as stand-alone diagnostic tools.
Implications for Clinical Practice
This review provides practical guidance to help healthcare professionals:
- Reassure families that infantile colic is usually a self-limiting condition
- Recognize that colic alone does not justify a diagnosis of CMA
- Identify clinical scenarios in which CMA may reasonably be suspected
- Apply a structured, time-limited elimination and reintroduction strategy when indicated
- Avoid unnecessary dietary restrictions, over-diagnosis of CMA, and inappropriate formula changes
Overall, the authors emphasize that CMA should be considered selectively rather than routinely in infants with colic, and only within the framework of established CMA diagnostic guidelines.
Access the full publication: https://doi.org/10.3390/nu17223600
Source
Nutrients, 2025
Vandenplas Y. et al.
DOI: 10.3390/nu17223600
